Author: Allison Tadros, MD, West Virginia University Department of Emergency Medicine
Editor: Matthew Tews, DO, MS, Medical College of Georgia at Augusta University
Objectives
- Describe the clinical decision rules to determine the indication for imaging in the emergency department
- Describe a method for systematically interpreting cervical spine imaging
- Recognize specific injuries related to cervical spine imaging
Clinical Decision-Making
When evaluating a patient with traumatic injury, one of several clinical decisions that must be made is whether or not imaging of the cervical spine is indicated. There are two validated decision rules that can be used to guide your decision, the Nexus criteria and the Canadian C spine rule.
Nexus Criteria
According to the NEXUS criteria, a patient undergoing trauma who meets all of the following criteria can have their c spine cleared clinically without imaging:
- No midline tenderness
- No pain with neck movement
- No distracting injury
- No neuro deficit
- No alcohol or drugs
- No altered mental status
Canadian Cervical Spine Rule
The Canadian C spine Rule can also be used to determine if c spine imaging is indicated. The Canadian C spine Rule is as follows:
Are any of the following present?
- Age older than 65 years
- Mechanism of injury considered dangerous
- Numbness or tingling present in the extremities
If yes, c spine imaging is indicated
If no, are any of the following low-risk indicators present?
- Simple rear-end motor vehicle collision
- Patient ambulatory at any time since injury
- Delayed onset of neck pain
- Patient in sitting position in emergency department
- Absence of midline cervical spine tenderness
If none are present, c spine imaging is indicated
If yes, is the patient able to look 45° in each direction?
If no, c spine imaging should be performed. If yes, c spine imaging is not necessary.
Choosing an Imaging Modality
When faced with injured patients, the healthcare provider must not only decide what parts of the body should be imaged, but also must decide which modality of imaging is most appropriate. One particularly challenging area is cervical spine imaging. In the past, computed tomography (CT) scan imaging of the cervical spine was reserved for better clarification of injuries seen on screening x-ray exams, or in cases when adequate images could not be obtained on x-rays (ex, non-visualization of junction of C7/T1). Subsequently a series of studies came out suggesting that x-rays were missing a significant number of injuries. Currently, CT has largely replaced plain radiographs of the cervical spine. However, more recent studies begin to shed light on the overuse of CT imaging, raising concerns over the cancer risk of ionizing radiation. Now the provider has to decide which patients are suitable for plain radiographs and in which cases CT imaging is more appropriate.
CT imaging of the c spine is thought to expose the patient to 5.7 mSv of radiation while an x ray series of the c spine exposes the patient to about 0.2 mSv. In addition, cervical imaging of all types exposes the radiation-sensitive thyroid gland to radiation. Although the guidelines mentioned previously assist in determining which trauma patients can have avoid the need for c spine imaging using clinical criteria, there are no guidelines or large studies to help us decide which imaging study to use. All of the studies touting CT as the better imaging modality did not take into consideration the risk of radiation exposure to the patient.
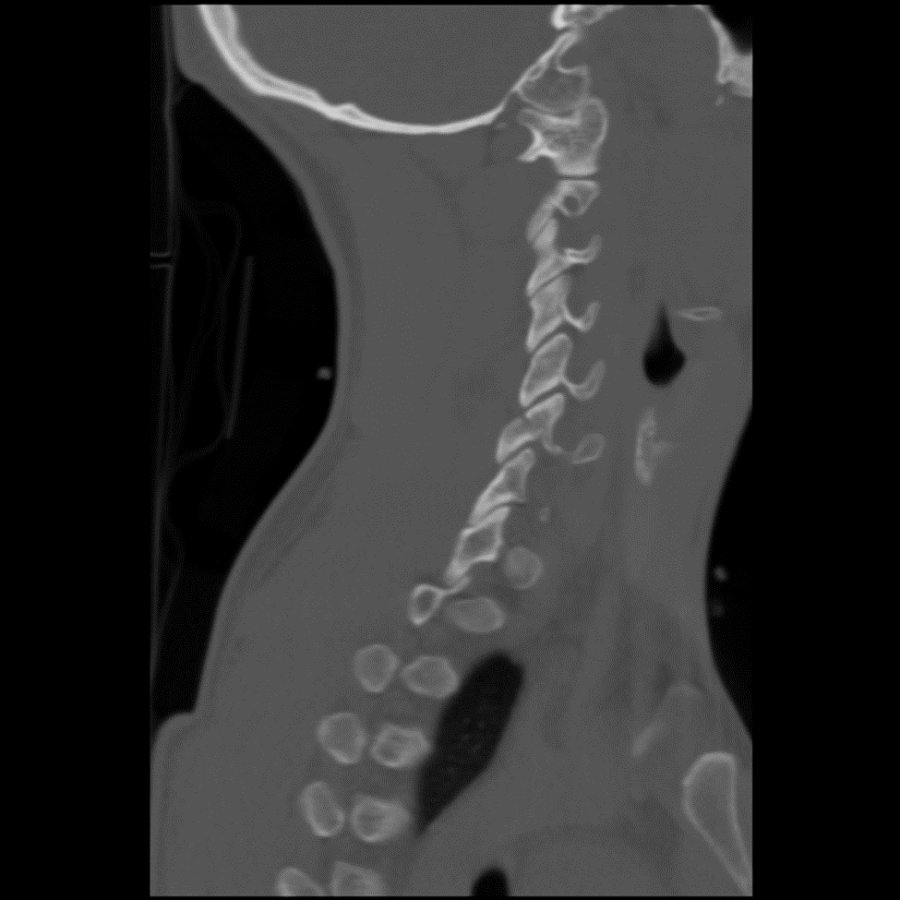
One of the factors that comes into consideration is determining what can be seen on a plain film x-ray versus a CT scan. Plain film x-rays may not demonstrate non-displaced injuries, which can then be seen on the more sensitive CT scan. For example, figures 1 and 2 are images from the same patient. Figure 1 is a lateral c spine radiograph that appears normal. Figure 2 is a sagittal reconstruction image of the c spine of the same patient that clearly demonstrates an oblique, non-displaced fracture traversing the left C6 superior and inferior facets.
Figure 1 Normal appearing lateral C spine
Figure 2 Sagital CT image of the same patient showing a fracture of C6
Another factor to consider is the age of the patient. Older patients have more degenerative changes to their spines which make it more difficult to interpret x rays. For example, loss of vertebral height could be age-related or could represent an acute compression fracture. If the radiologist is unable to differentiate between the two, a CT may be recommended. This will expose the patient to even more radiation as well as higher cost and length of stay in the emergency department than would occur if the CT had been ordered originally. In addition, radiation exposure is more of a concern in the younger patient. Therefore, an older patient with neck pain after a fall or MVC should probably undergo CT imaging compared to x-rays when imaging is indicated
A patient with neurologic deficits, who is obtunded, or who has significant other injuries is more at risk of having a c spine injury. Therefore, patients falling into these categories probably deserve CT imaging when cervical spine injury is suspected or based on reported mechanism. For patients who are unable or unwilling to cooperate with x-ray imaging, CT imaging may be a better option to better characterize the injury.
In the case of young patients in whom there is a low clinical suspicion for significant injury, but who meets the criteria for imaging based upon the presence of midline neck tenderness, it seems reasonable to order x rays to try to avoid the CT scan. If the x rays are negative, it is appropriate to discharge the patient in a cervical collar with a follow up in one 1 week for reassessment if they continue to have pain.
Approach to Interpreting Cervical Spine Imaging
Once imaging is obtained, it is useful to have a systematic approach for reviewing the images. While a radiologist will eventually read the film, the provider in the emergency department should be able to review the films and correlate areas of pain with the imaging. A useful tool to recall is the ABCS method.
ABCs of Cervical Spine Imaging Evaluation
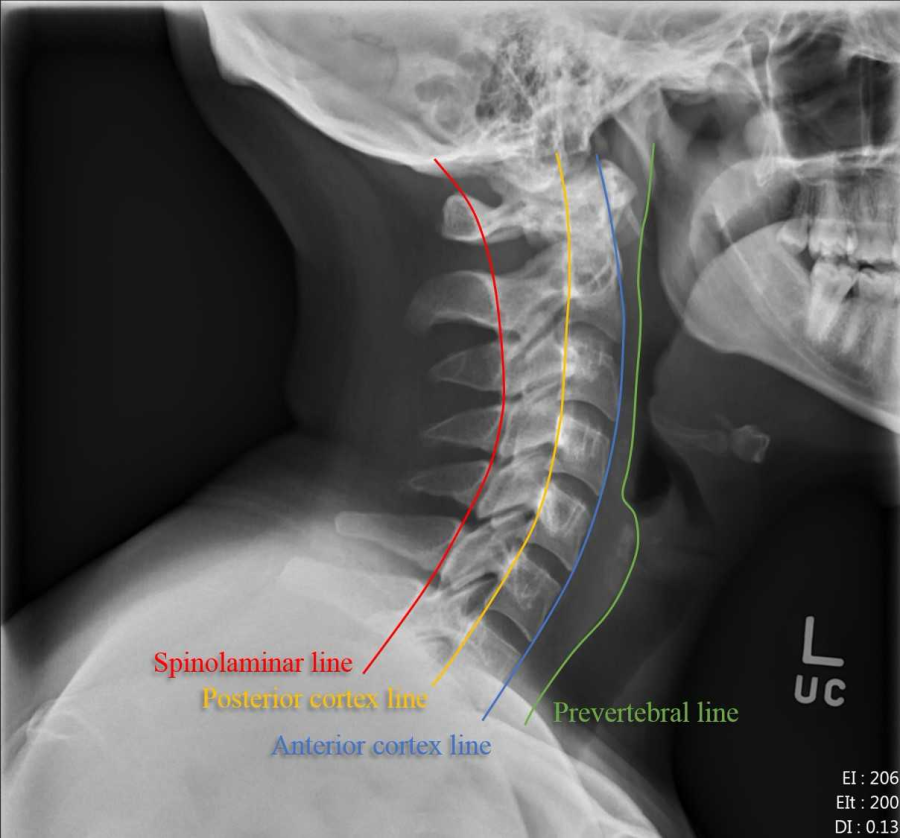
A – Alignment & Anatomy
B – Bony integrity
C – Cartilage (Joint) spaces
S – Soft Tissues
A – Alignment & Anatomy
- Visually trace the 4 lines labelled in Figure 3
- Look for disrupted anterior or posterior vertebral body lines.
- Look for disruption of the spinolaminar line
- Look for asymmetry of the facets
- Look for widening of the spaces between the individual vertebrae
- Look for widened the predental soft tissue space
B – Bony abnormalities
- Overt fracture lucencies/deformities
- Once one fracture is seen, be sure to look for others
- Disruption of the ring of C1 (Odontoid Fx)
C – Cartilage (Joint) abnormalities
Widened or narrowed disc space/facets
S – Soft tissue abnormalities
- Widened prevertebral space
- >7mm should prompt high suspicion for injury
Figure 3 Lateral C spine radiograph with 4 anatomic lines
Mechanisms of Trauma to the Cervical Spine
There are six simplified forces that are applied to the cervical spine during trauma which should be considered and correlated to the imaging. Most injuries are a combination of these forces, but injuries seen on imaging can be further understood when seen:
- Flexion
- Extension
- Distraction
- Rotation
- Compression
- Shearing
| Mechanism | Example Injuries |
| Flexion
|
Hyperflexion sprain
Bilateral interfacetal dislocation Simple compression fracture Clay shoveler’s fracture (spinous process fracture of C6 or C7) Flexion teardrop fracture |
| Extension
|
Hyperextension Dislocation
Extension Teardrop Fracture Hangman’s Fracture Laminar Fractures |
| Rotation
|
Results in disruption of interspinous ligaments.
Fractures of spinous processes, facets (dislocations), and laminae. Rarely occurs in isolation; usually associated with flexion mechanism. Unilateral Interfacetal Fracture/Dislocations most important injury. |
| Compression
|
All three columns subjected to axial load.
Rarely occurs in isolation Vertebral endplate is the site of the majority of force (due to intervertebral disc). With enough force, disc is forced into vertebral body leading to axial displacement of fragments (burst fracture). Retropulsion of fragments into spinal canal. Example injuries: Jefferson Fracture of C1 Burst Fracture of Lower C-spine |
Specific injuries
Bilateral Interfacetal Dislocation (BID)- Figures 4 and 5
- Predominantly a soft tissue (ligament) injury
- Almost all of the supporting ligaments are injured
- This fracture is completely unstable and has a high incidence of cord injury
- Imaging findings:
- Both facets dislocated
- Complete (‘jumped’) or incomplete (‘perched’) facets
- Focal kyphotic angulation
- Anterior dislocation of superior vertebral body
Figure 4 Bilateral interfacet dislocation on plain radiograph
Figure 5 Bilateral interfacet dislocation on sagittal CT image
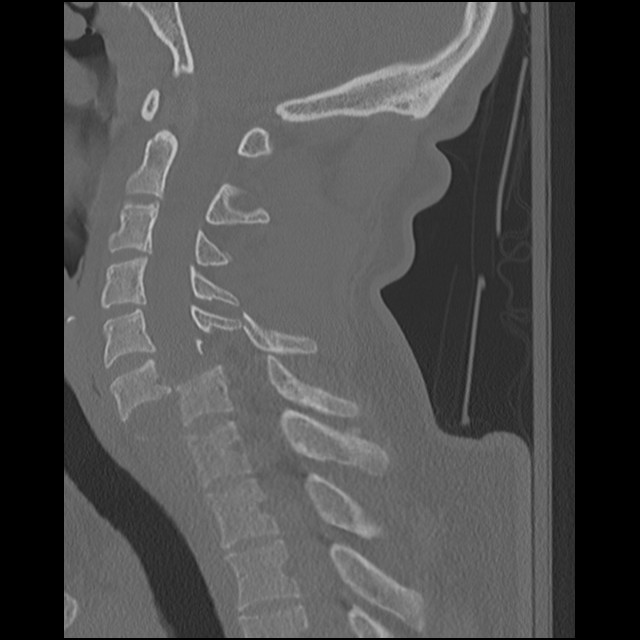
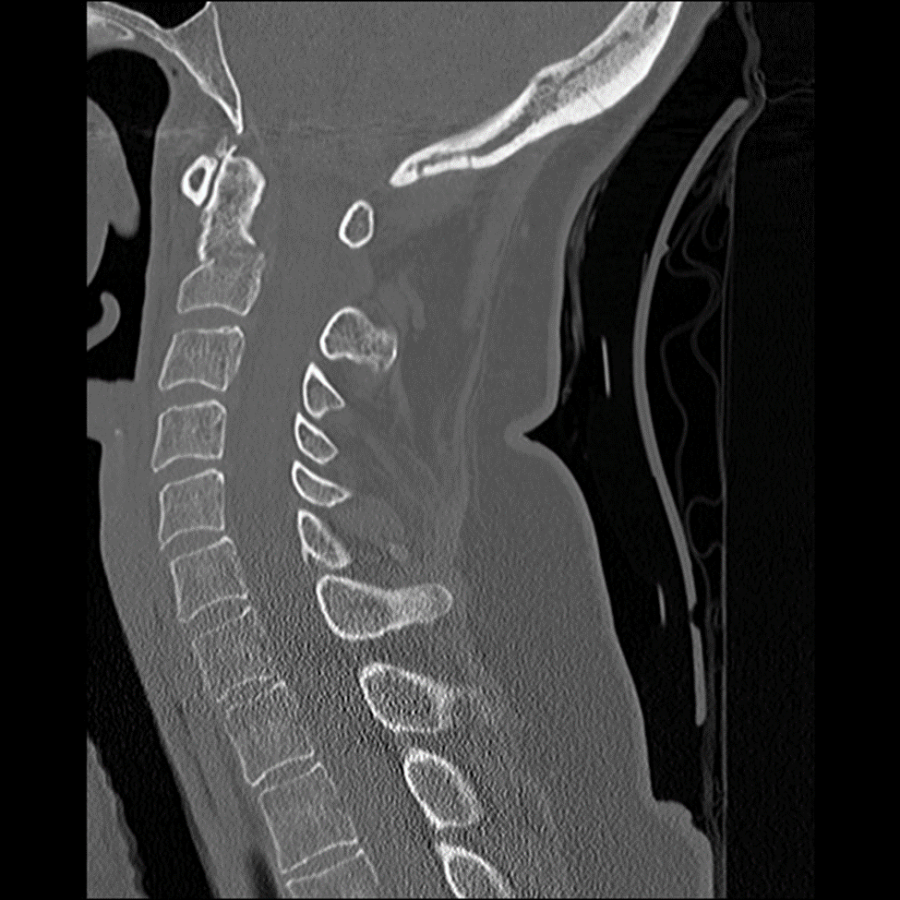
Traumatic Spondylolisthesis (Hangman’s Fracture)
- Fx of the bilateral pars interarticularis of C2
- This fracture is considered unstable, though neurologic deficit is rare
- Large size of canal relative to cord
- Auto-decompression with bilateral fractures
- Imaging findings:
- Best seen on lateral view and CT.
Figure 6 Hangman’s fracture of C2 on plain radiograph
Figure 7 Hangman’s fracture on sagittal CT
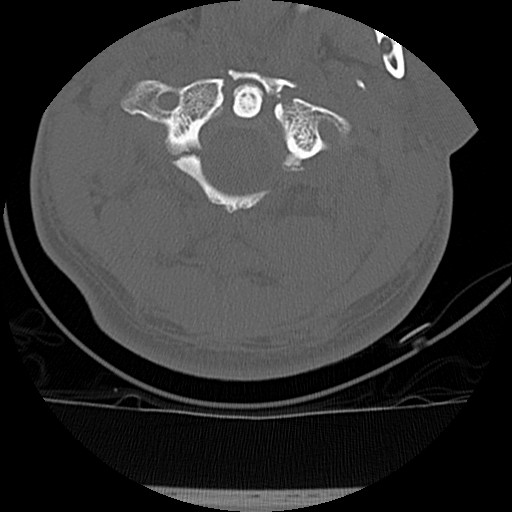
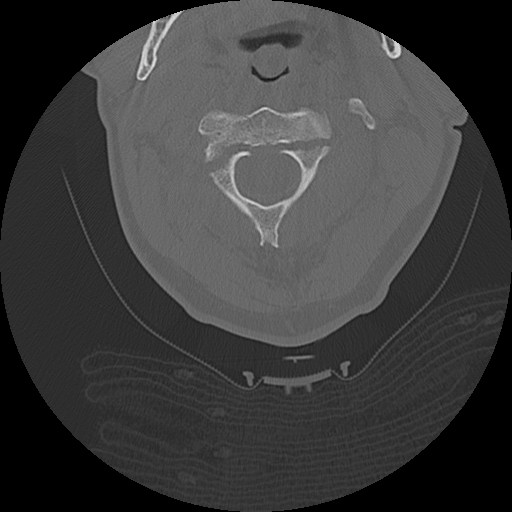 Figure 8 Hangman’s fracture on CT axial image
Figure 8 Hangman’s fracture on CT axial image
Jefferson Fracture
- Vertical force transmitted from skull vertex to occipital condyles to lateral masses of C1
- Disruption of both anterior and posterior arches
- Stability depends on integrity of transverse ligament
- Greater than 7 mm of TOTAL bilateral offset implies instability
- Imaging findings:
- Lateral displacement of lateral masses of C1 (open mouth)
- Posterior arch fractures (lateral view)
- Cervicocranial prevertebral swelling
Figure 9 Jefferson fracture of C1 on plain radiograph
Figure 10 Jefferson fracture of C1 on axial CT image
Unilateral Interfacetal Dislocation (UID)
- Hyperflexion-Rotation injury
- Superior facet dislocated superior and anterior to adjacent inferior facet
- This fracture is considered stable, displaced facet adds to stability
- Imaging findings:
- One facet dislocated
- Anterior dislocation of superior vertebral body <½ width of inferior vertebral body
- Rotation of levels above injury
- Splaying of interspinous space
Figure 11 Unilateral Interfacetal Dislocation on axial CT
Figure 12 Unilateral Interfacetal Dislocation on sagittal CT image
Flexion Teardrop Fracture
- Most severe survivable C-spine injury.
- All three columns completely disrupted (unstable)
- Imaging findings:
- Severe flexion deformity at/above injury level
- ‘Teardrop’ fracture fragment off anterior inferior corner
- Posterior subluxation/dislocation of fractured vertebra
- Widening of interspinous space
Odontoid Fractures
There are 3 types of fracture patterns based on the Anderson and d’Alonzo classification
- Type I: oblique fracture of tip of dens (probably doesn’t exist)
- Type II: transverse fracture at base of dens (66%)
- 64-100% non-union
- Unstable (cephalad fragment and C1 move together)
- Type III: oblique fracture into body of C2 (30%)
- High union rate (cancellous bone)
- Unstable
Figure 13 Type 3 Odontoid Fracture on lateral plain radiograph
Figure 14 Type 3 Odontoid Fracture on CT sagittal image
Figure 15 Type 3 Odontoid Fracture on CT coronal image
Pearls
- Have a low threshold for imaging the cervical spine and use a decision rule to determine who can have their cervical spine cleared clinically following trauma.
- Consider if if your patient is a candidate for plain radiographs instead of CT, particularly if their pain is mild, their traumatic mechanism was low risk, and they are young.
- Develop a systematic approach to reviewing images of the cervical spine, looking for fractures, soft tissue swelling, symmetry, and alignment.
Conclusion
In conclusion, there is little evidence-based medicine to guide the health care provider on what population of trauma patients can be safely evaluated by plain radiographs of the c spine alone. There is plenty of literature that tells us that radiographs will miss injuries that are seen on CT scan. On the other hand, there is growing evidence that the volume of imaging studies we are ordering, particularly CT imaging, is harmful to patients. Until a large, well-designed study is conducted to provide guidance on which modality to order, use the validated clinical decision rules and clinical judgement to determine what to order. When reviewing the films, use a systematic approach to reading the images. It is important to be aware of the mechanism of injury as it correlates with the imaging findings; be aware of the unstable fracture patterns.
References
- Emergency department evaluation and treatment of cervical spine injuries.Kanwar R, Delasobera BE, Hudson K, Frohna W, 1. Emerg Med Clin North Am. 2015 May;33(2):241-82. doi: 10.1016/j.emc.2014.12.002. Epub 2015 Mar 14
- The Canadian C-spine rule for radiography in alert and stable trauma patients. Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ, Laupacis A, Schull M, McKnight RD, Verbeek R, Brison R, Cass D, Dreyer J, Eisenhauer MA, Greenberg GH, MacPhail I, Morrison L, Reardon M, Worthington J., JAMA. 2001 Oct 17;286(15):1841-8.
- Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group., Hoffman JR1, Mower WR, Wolfson AB, Todd KH, Zucker MI. N Engl J Med. 2000 Jul 13;343(2):94-9.
- Imhof H. (2007) Imaging of Spinal Injuries. In: Marincek B., Dondelinger R.F. (eds) Emergency Radiology. Springer, Berlin, Heidelberg
- Daffner, R, Harris, J (2012) C spine Injuries. In: Harris & Harris’ The Radiology of Emergency Medicine. Wolters Kluwer Health
Credits
All images are courtesy of Dr William Krantz, West Virginia University, Department of Radiology, and are used with permission.